Non-immune hydrops fetalis (NIHF) can be one of the earliest signs of MPS VII1,2
MPS VII often goes undiagnosed in fetal-stage infants with idiopathic NIHF3
Hydrops fetalis is a life-threatening fetal state that is characterized by increased fluid accumulation in fetal soft tissues and body cavities. It can be diagnosed in utero or postnatally.3
Specifically, non-immune hydrops fetalis4
- Accounts for ~90% of cases of hydrops, with an incidence of 1 in 1700 to 3000 pregnancies, and has many causes
- Has been reported as idiopathic in older studies, but recent larger studies and a systematic review report that a cause can be found in up to 85% of cases
About 70% of the time, NIHF clinical workups did not test for lysosomal storage disorders (LSDs) like MPS VII.4
The NIHF and MPS VII correlation has historically been under recognized1,4
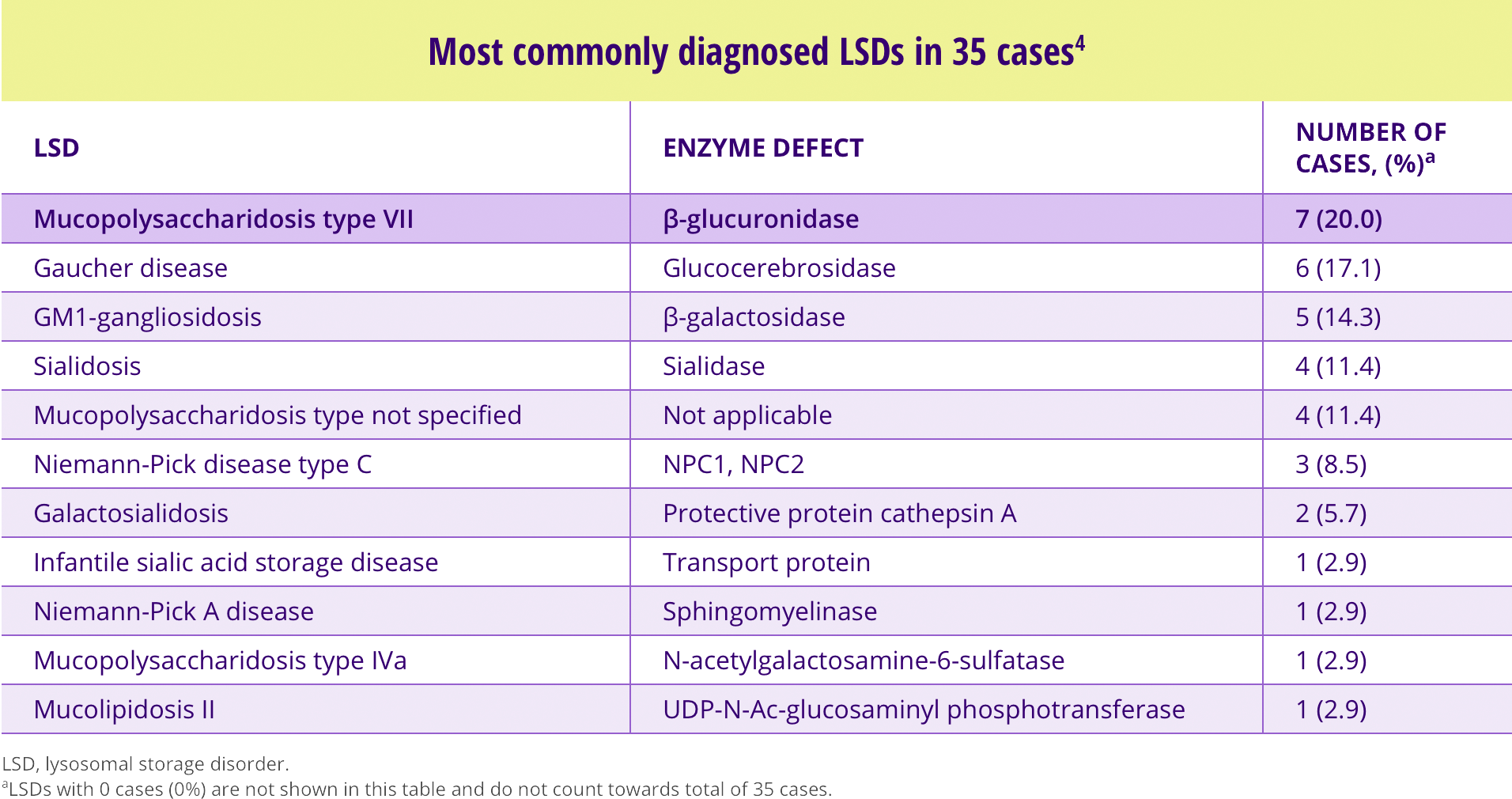
- MPS VII is the most commonly diagnosed LSD in cases of NIHF 4
- ~40% of MPS VII patients have a history of NIHF, from a survey of 118 patients in 25 countries1

Matthew’s story
Matthew’s story
Matthew, born prematurely at 34 weeks with multiple health concerns, was found by doctors to have non-immune hydrops fetalis (NIHF). At 18 months of age, he became one of the very few children to be diagnosed with both NIHF and MPS VII.
Despite challenges, he has learned sign language and is eager to learn more. A popular child at the rehabilitation facility where he lives, his smile and happy demeanor have left an imprint on all who care for him. Matthew’s strength and fighting spirit continue to inspire us all.
A literature analysis reporting cases of NIHF from 1979 to 2014 was performed to4
A literature analysis reporting cases of NIHF from 1979 to 2014 was performed to4
- Evaluate the significance of LSDs as an underlying etiology of NIHF
- Determine whether identifying LSDs would be clinically useful in the workup of NIHF
Of the 678 total NIHF cases identified
- 5.2% (35) were diagnosed with LSD
- 70.3% (477) had a diagnosis other than LSD
- 24.5% (166) were idiopathic
Importance of comprehensive testing4
LSDs have been reported to account for about 1%-15% of the causes of NIHF cases. Yet in clinical practice, these LSDs are often not evaluated.
A literature analysis found that of the 18%-30% of cases in which the initial NIHF workup did not reveal a probable etiology
- Testing for LSDs resulted in a diagnosis in 17.4% of cases
- Evidence supports an estimate that 29.6% of those cases that would have been classified as idiopathic would have had a diagnosis of LSD
- The more common positive LSDs were mucopolyaccharidosis type VII, Gaucher disease, and GM1-gangliosidosis
Based on the literature analysis, a 2-step approach is recommended for identifying LSDs as a cause of NIHF4:

Common causes of NIHF should be evaluated

For cases that remain idiopathic after the initial NIHF workup, comprehensive testing for LSDs
should be done
 English
English  English, UK
English, UK Español
Español Português
Português Italiano
Italiano Hrvatski
Hrvatski Magyar
Magyar Polski
Polski Română
Română



